This is an update to a story I wrote five years ago, for Johns Hopkins Rheumatology’s LEAP Magazine, with two world experts on PTLD: post-treatment Lyme disease. They have uncovered some promising clues as to why, for some people, Lyme disease doesn’t go away, and identified some new potential avenues of treatment.
Some people get bitten by a deer tick that’s infected with Borrelia burgdorferi, develop a rash, are diagnosed with Lyme disease, take antibiotics, feel better, and get their life back to normal.
Others aren’t so lucky. Diagnosed just as promptly, they take the exact same course of antibiotics. And then… they don’t get better. What’s happening?
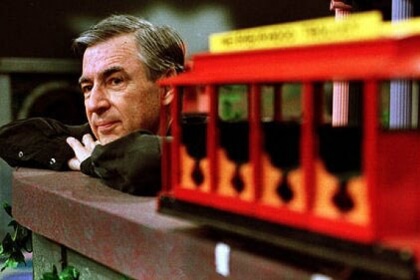
John Aucott, M.D., an infectious diseases specialist and the founding Director/physician of the Johns Hopkins Lyme Disease Research Center, is a world authority on this “post-treatment Lyme disease” (PTLD), a condition he helped define. Its symptoms are persistent, and can include fatigue, pain, weakness, brain fog, and sleep disorders. He has studied and treated hundreds of patients with PTLD, who tell him things like, “I can’t get out of bed,” or “I can’t ride my bike,” or “I’m exhausted trying to get through the work day.” In addition to feeling ill, frustrated, discouraged and even desperate for relief, these patients often must deal with a stigma – similar to that experienced by a brand-new group of patients from the pandemic, the Covid-19 ‘long-haulers,’ Aucott says. “The Covid long-haulers aren’t dying, they don’t have signs of extensive organ damage – but they have the exact same lingering, disabling symptoms that we have been pointing out for years in our PTLD patients.”
Aucott and his longtime colleague, scientist Mark Soloski, Ph.D., suspect that for the PTLD “long-haulers” – about 10 to 15 percent of people treated for acute (initial) Lyme disease – the disease process triggers persistent changes in the immune system and the autonomic nervous system. Their pioneering research program focuses on defining and characterizing changes in the underlying molecular mechanisms that cause and perpetuate these symptoms, with the hope of finding biomarkers to help diagnose and monitor this disease, and to discover new avenues of treatment. Their areas of active study include:
The gut microbiome: In work recently published online in mBio, Soloski, Aucott and colleagues at Hopkins, Northeastern University, and University of California-San Diego reported that PTLD patients have a distinct microbiome “signature,” or population of bacteria in their gastrointestinal tract compared to healthy controls and to an intensive care unit control group. The scientists analyzed fecal samples from patients in the Hopkins Study of Lyme Immunology and Clinical Endpoints (SLICE), and compared them to a healthy control group and to an intensive care unit (ICU) control group – patients who were also on antibiotics. “We found that the PTLD group had two distinct differences in their gut bacteria – an abundance of Blautia bacteria, and a decrease in Bacteroides,” says Soloski. “Bacteroides is interesting, because it produces GABA, an important neurotransmitter.” Low levels of GABA can cause anxiety and depression. In turn, an excess of Blautia has been found in people with obesity, Alzheimer’s disease, and multiple sclerosis. The good news about the gut microbiome is that it can be altered by many factors, including diet, medication, and even fecal transplant. It may be that reintroducing healthy bacteria into the colon could significantly improve quality of life in these patients – a compelling idea that the investigators feel is worthy of further study.
The metabolic response: In another study, Soloski, Aucott and colleagues at Hopkins, the centers for Disease Control, Colorado State University, and New York Medical College found significant metabolic differences in people with PTLD compared to other patients. This work was published in Clinical Infectious Diseases. “Basically, we found that the metabolome – all those small molecules our cells make and pour out into our blood, our signature of the metabolic activities of all the cells in the body – is perturbed in patients with Lyme disease.” The scientists have identified a “fingerprint” of metabolites unique to patients with PTLD. This might one day lead to a blood test to determine which patients with Lyme disease are at risk of PTLD, and to help monitor the course of illness in PTLD patients.
Is there a genetic fingerprint? Soloski and Aucott are looking for epigenetic changes – small mutations in the structure of DNA – among the 20,000 or so genes in the genome. This is big-data analysis that wouldn’t have been possible a few years ago. Computers and data experts sift countless pieces of evidence, like miners sluicing for gold, looking for valuable nuggets: patterns of gene expression, particularly in immune system genes and in messenger RNA genes.
Not Always a Bullseye
Artificial intelligence (AI) is making possible what John Aucott describes as his “pet project:” analyzing the rash that comes at the start of Lyme disease and is key to early diagnosis. “Our studies show that many people have trouble making the right diagnosis. Everybody’s looking for the Target store sign,” but that distinctive bullseye only appears in 20 percent of patients. “Patients and clinicians miss the other 80 percent. We trained the computer by AI to read cell phone images and make a better diagnosis.” Aucott was senior author on a report of this work, recently published in Computers in Biology and Medicine.
Could rashes even help predict which patients might be headed for PTLD, and could a better understanding of rashes lead to more effective, personalized treatments? These are possibilities Aucott hopes to explore.
Better treatment for PTLD
“There is no FDA-approved treatment for PTLD,” says Aucott, “so we use drugs that the FDA has approved for other indications. Treatment is very patient-specific, depending on the primary symptoms.” For example, fatigue often goes along with postural orthostatic tachycardia syndrome (POTS), a condition where the heartbeat skyrockets with a change of position – from sitting to standing, for example – that is treated by blood pressure-regulating drugs such as midodrine.
In exciting research recently published online in BMJ Open, Hopkins scientists Alison Rebman, Ting Yang, and Aucott, have identified six symptom factors and three potentially clinically relevant subgroups among patients with PTLD. The group’s findings may be an important step toward developing even more personalized and specific treatment plans.
Aucott has spent years working to raise physician awareness about PTLD, which “doesn’t fit into one specific disease silo” or subspecialty; in fact, the Center is the only one of its kind based in an academic department of medicine in the world with a focus on PTLD.
New to the Center is rheumatologist John Miller, M.D., who brings expertise in joint ultrasound. “He is showing changes in our patients that are subtle,” particularly “tendinopathy-related causes of periarticular pain that nobody’s seen before, because joint ultrasound has never been done in these patients.” Miller has found enthesitis, inflammation where tendons insert into the joints that is also found in psoriatic arthritis and Reiter’s syndrome (reactive arthritis). His findings “may lead to looking at autoimmune-related drugs,” says Aucott, and the images “are opening up a whole new field of clinical inquiry. Nobody else is really doing this.”
You can learn more about the Center here.
©Janet Farrar Worthington

 This is what doctors at the Amos Center for Food, Body & Mind at Johns Hopkins Bayview Medical Center want to know.
This is what doctors at the Amos Center for Food, Body & Mind at Johns Hopkins Bayview Medical Center want to know.
 It’s important to remember that “the microbiome is just part of the study,” Harer continues.
It’s important to remember that “the microbiome is just part of the study,” Harer continues.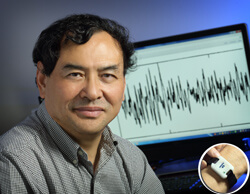

 Yogurt. Look for the words, “Live and active cultures.” These are probiotics, and besides increasing the number of good bacteria in your gut, they can help reduce symptoms of irritable bowel syndrome, and also can help improve symptoms of inflammatory bowel diseases, such as Crohn’s and ulcerative colitis. Greek yogurt has more protein than traditional yogurt; it takes longer to digest and can help you feel full longer — which, in turn, can reduce the need for snacks between meals, so as a bonus, it may help you lose weight.
Yogurt. Look for the words, “Live and active cultures.” These are probiotics, and besides increasing the number of good bacteria in your gut, they can help reduce symptoms of irritable bowel syndrome, and also can help improve symptoms of inflammatory bowel diseases, such as Crohn’s and ulcerative colitis. Greek yogurt has more protein than traditional yogurt; it takes longer to digest and can help you feel full longer — which, in turn, can reduce the need for snacks between meals, so as a bonus, it may help you lose weight.